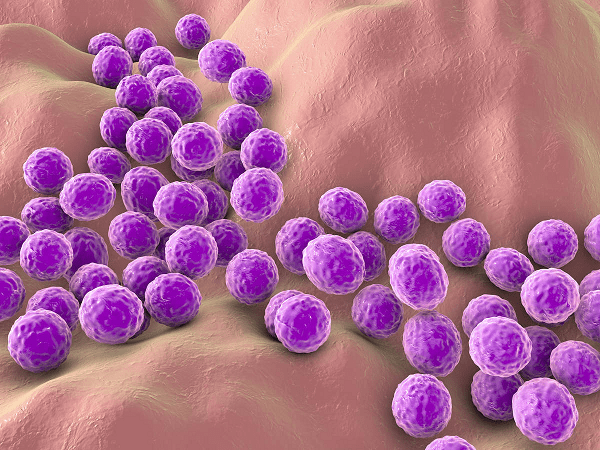
Staphylococci- Staphylococci, often referred to as staph bacteria, are a group of Gram-positive bacteria that belong to the family Staphylococcaceae. They are spherical in shape and typically occur in clusters, resembling grapes under a microscope. Staphylococci are commonly found on the skin and mucous membranes of humans and animals.
There are various species of staphylococci, but Staphylococcus aureus and Staphylococcus epidermidis are among the most well-known and clinically significant:
- Staphylococcus aureus (S. aureus):
- S. aureus is a versatile and opportunistic pathogen that can cause a wide range of infections in humans.
- It is known for causing skin and soft tissue infections, such as boils, cellulitis, and impetigo, as well as more serious conditions like pneumonia, bloodstream infections (bacteremia), and endocarditis.
- Some strains of S. aureus have developed resistance to multiple antibiotics, leading to the emergence of methicillin-resistant Staphylococcus aureus (MRSA), which can be difficult to treat.
- Staphylococcus epidermidis (S. epidermidis):
- S. epidermidis is a commensal bacterium that normally resides on human skin and mucous membranes.
- While it is typically harmless, S. epidermidis can be opportunistic and cause infections in people with weakened immune systems or implanted medical devices. It is a common cause of infections associated with catheters, prosthetic joints, and other medical devices.
Staphylococci are known for their ability to survive in a variety of environments and resist desiccation, making them resilient on surfaces and medical equipment. They can also produce toxins and enzymes that contribute to their pathogenicity.
Treatment of staphylococcal infections often involves antibiotics, but the choice of antibiotic depends on the specific strain of staph bacteria and its susceptibility to drugs. In the case of MRSA, treatment options may be limited due to antibiotic resistance, and alternative therapies may be required.
Preventative measures, such as good hand hygiene, proper wound care, and the appropriate use of antibiotics, are important in reducing the risk of staphylococcal infections, especially in healthcare settings.
What is Staphylococci
Staphylococci, often referred to as staph bacteria, are a group of Gram-positive bacteria that belong to the family Staphylococcaceae. They are spherical in shape and typically occur in clusters, resembling grapes under a microscope. Staphylococci are commonly found on the skin and mucous membranes of humans and animals.
There are various species of staphylococci, but Staphylococcus aureus and Staphylococcus epidermidis are among the most well-known and clinically significant:
- Staphylococcus aureus (S. aureus):
- S. aureus is a versatile and opportunistic pathogen that can cause a wide range of infections in humans.
- It is known for causing skin and soft tissue infections, such as boils, cellulitis, and impetigo, as well as more serious conditions like pneumonia, bloodstream infections (bacteremia), and endocarditis.
- Some strains of S. aureus have developed resistance to multiple antibiotics, leading to the emergence of methicillin-resistant Staphylococcus aureus (MRSA), which can be difficult to treat.
- Staphylococcus epidermidis (S. epidermidis):
- S. epidermidis is a commensal bacterium that normally resides on human skin and mucous membranes.
- While it is typically harmless, S. epidermidis can be opportunistic and cause infections in people with weakened immune systems or implanted medical devices. It is a common cause of infections associated with catheters, prosthetic joints, and other medical devices.
Staphylococci are known for their ability to survive in a variety of environments and resist desiccation, making them resilient on surfaces and medical equipment. They can also produce toxins and enzymes that contribute to their pathogenicity.
Treatment of staphylococcal infections often involves antibiotics, but the choice of antibiotic depends on the specific strain of staph bacteria and its susceptibility to drugs. In the case of MRSA, treatment options may be limited due to antibiotic resistance, and alternative therapies may be required.
Preventative measures, such as good hand hygiene, proper wound care, and the appropriate use of antibiotics, are important in reducing the risk of staphylococcal infections, especially in healthcare settings.
Who is Required Staphylococci
“Staphylococci” is not a person or an individual; it’s a term used to describe a group of bacteria known as Staphylococcus. Staphylococcus is a genus of Gram-positive bacteria that are commonly found on the skin and mucous membranes of humans and animals. They are characterized by their spherical shape and the tendency to form clusters, resembling grapes under a microscope.
Staphylococcus bacteria can include various species, with Staphylococcus aureus and Staphylococcus epidermidis being two of the most well-known species within this genus. These bacteria can sometimes cause infections in humans, ranging from minor skin infections to more serious conditions like pneumonia, bloodstream infections, and endocarditis. Staphylococcus aureus, in particular, can be responsible for a wide range of infections and is known for its ability to develop antibiotic resistance, leading to the emergence of MRSA (methicillin-resistant Staphylococcus aureus).
If you have a specific question about Staphylococcus or a related topic, please feel free to ask, and I’ll do my best to provide you with more information.
When is Required Staphylococci
I apologize, but the phrase “Required Staphylococci” does not appear to have a recognized or standard meaning in microbiology, medicine, or any other field. It is not clear what you are referring to with this specific term.
If you have a question or need information about a particular topic related to Staphylococcus bacteria or any other subject, please provide more context or clarify your question, and I will be happy to assist you to the best of my ability.
Staphylococci, which are a group of bacteria belonging to the genus Staphylococcus, are not associated with specific dates or times. They are microorganisms that can be found on the skin and mucous membranes of humans and animals at any time, and their presence is not tied to a specific calendar date.
If you have a specific question about Staphylococcus bacteria or a related topic, please provide more details or clarify your question, and I’ll be happy to assist you further.
Where is Required Staphylococci
Staphylococci, specifically Staphylococcus bacteria, can be found in various locations, primarily on the skin and mucous membranes of humans and animals. Here are some common places where Staphylococci can be found:
- Skin: Staphylococci are part of the normal flora of the skin, and they can be found in the sweat glands, hair follicles, and other areas of the skin’s surface.
- Nasal Passages: Staphylococci, especially Staphylococcus aureus, can colonize the nasal passages of some individuals.
- Mouth and Throat: Staphylococci may also be present in the oral cavity and throat, though they are not as commonly found there as other types of bacteria.
- Mucous Membranes: These bacteria can inhabit various mucous membranes throughout the body, including the respiratory, gastrointestinal, and genitourinary tracts.
- Hospital Environments: Staphylococci, particularly Staphylococcus aureus, can be found on surfaces, medical equipment, and in healthcare settings, posing a risk for healthcare-associated infections.
- Environmental Surfaces: Staphylococci can survive on various surfaces, including clothing, towels, and household items, though their presence in the environment is generally lower than on human skin.
It’s important to note that while Staphylococci are part of the normal flora in many individuals and can be harmless, some strains of Staphylococcus, such as Staphylococcus aureus, can cause infections when they enter the body through cuts, wounds, or other entry points. Additionally, the presence of Staphylococci in healthcare settings can be a concern due to the potential for healthcare-associated infections, especially when proper hygiene and infection control measures are not followed.
How is Required Staphylococci
Staphylococci, specifically the bacteria of the genus Staphylococcus, are microorganisms that can be characterized in various ways, including their morphology, growth conditions, and behavior. Here is how Staphylococci are generally described:
- Morphology: Staphylococci are Gram-positive bacteria, which means they have a thick layer of peptidoglycan in their cell walls, retaining a violet stain when subjected to Gram staining. They are typically spherical or round in shape and often occur in clusters, resembling bunches of grapes under a microscope.
- Growth Conditions: Staphylococci are facultative anaerobes, which means they can grow both in the presence and absence of oxygen. They thrive in a wide range of environments, including on the skin and mucous membranes of humans and animals. Some species are also capable of surviving in various environmental conditions.
- Nutrition: Staphylococci are heterotrophic bacteria, meaning they obtain nutrients by breaking down organic molecules. They can utilize a variety of carbon and energy sources, allowing them to grow on different types of organic matter.
- Pathogenicity: While some species of Staphylococcus are part of the normal flora of the human body and are harmless, others can be opportunistic pathogens. Staphylococcus aureus, in particular, is known for causing a range of infections in humans, from skin and soft tissue infections to more severe systemic illnesses. Some strains of Staphylococcus aureus have developed antibiotic resistance, such as MRSA (methicillin-resistant Staphylococcus aureus), making them challenging to treat.
- Toxin Production: Staphylococci can produce various toxins and enzymes, such as coagulase, hemolysins, and enterotoxins. These virulence factors can contribute to their pathogenicity and the severity of infections they cause.
- Identification: In a laboratory setting, Staphylococci can be identified through techniques like Gram staining, culture on specific agar plates, and biochemical tests. Molecular techniques like polymerase chain reaction (PCR) may also be used for precise identification and strain typing.
- Treatment: Infections caused by Staphylococci are typically treated with antibiotics. However, the choice of antibiotics depends on the specific species and its susceptibility to drugs. Due to antibiotic resistance, especially with MRSA strains, choosing the right antibiotic can be crucial for successful treatment.
It’s important to note that Staphylococci are a diverse group of bacteria with various species, and their characteristics can vary between species and strains. Some are harmless colonizers of the skin and mucous membranes, while others can cause infections, so their impact on human health can vary widely.
Case Study on Staphylococci
Staphylococcus aureus Skin Infection
Patient Information:
- Name: John
- Age: 35
- Gender: Male
- Medical History: No significant medical history or known allergies
- Presenting Complaint: Painful skin lesion on his forearm
Clinical Presentation: John arrives at the emergency room with a painful red and swollen area on his right forearm. He reports that the lesion appeared a few days ago and has been getting progressively worse. He describes the pain as sharp and localized. The area is warm to the touch, and there is a visible central pustule (a raised, pus-filled blister).
Initial Assessment: Upon examination, the healthcare provider notes the following:
- Erythema (redness) and swelling around the lesion.
- A visible pustule in the center of the affected area.
- Tenderness to palpation (touch).
- No signs of fever or systemic illness.
- No known recent injuries or trauma to the area.
Diagnostic Steps:
- Swab Sample: The healthcare provider decides to take a swab sample from the lesion. This sample will be sent to the laboratory for microbiological analysis.
- Laboratory Analysis: In the lab, the swab sample is subjected to various tests:
- Gram Staining: The Gram stain reveals Gram-positive cocci in clusters, consistent with Staphylococcus.
- Culture and Sensitivity: The sample is cultured on agar plates. After incubation, colonies with characteristics of Staphylococcus aureus are identified.
- Antibiotic Susceptibility Testing: Susceptibility testing is performed to determine which antibiotics are effective against the isolated Staphylococcus aureus strain.
Diagnosis: The laboratory results confirm the presence of Staphylococcus aureus in the lesion. Additionally, antibiotic susceptibility testing shows that the strain is methicillin-sensitive Staphylococcus aureus (MSSA).
Treatment: Based on the diagnosis and susceptibility results, the healthcare provider prescribes antibiotics to treat the infection. In this case, oral antibiotics such as dicloxacillin or cephalexin, which are effective against MSSA, are prescribed for a specific duration.
Follow-Up: John is instructed to take the prescribed antibiotics as directed and to keep the affected area clean and dry. He is advised to return for a follow-up appointment in a week to monitor the progress of the infection.
Outcome: With appropriate treatment, the Staphylococcus aureus skin infection gradually improves. John experiences a reduction in pain, swelling, and redness over the course of his antibiotic treatment. At the follow-up appointment, the healthcare provider confirms that the infection has resolved, and John is advised to complete the full course of antibiotics.
This case study demonstrates a common clinical scenario involving a Staphylococcus aureus skin infection and the steps taken for diagnosis and treatment. Staphylococcus aureus skin infections can vary in severity, and proper diagnosis and treatment are essential to ensure a favorable outcome for the patient.
White paper on Staphylococci
Table of Contents
- Introduction
- Brief overview of Staphylococci
- Importance of studying Staphylococci
- Taxonomy and Classification
- Explanation of the genus Staphylococcus
- Common species within the genus
- Morphology and Structure
- Description of the typical characteristics of Staphylococci
- Microscopic appearance and colony morphology
- Ecology and Distribution
- Where Staphylococci are commonly found
- Commensalism vs. pathogenicity
- Pathogenic Staphylococci
- Staphylococcus aureus: Characteristics and virulence factors
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Other pathogenic species
- Clinical Manifestations
- Skin and soft tissue infections
- Respiratory infections
- Bacteremia and endocarditis
- Toxin-mediated illnesses
- Epidemiology
- Prevalence and incidence of Staphylococcal infections
- Risk factors for infection
- Diagnosis
- Microbiological techniques for identification
- Antibiotic susceptibility testing
- Treatment
- Antibiotics commonly used to treat Staphylococcal infections
- Challenges of antibiotic resistance
- Prevention and Infection Control
- Strategies to prevent Staphylococcal infections
- Infection control practices in healthcare settings
- Current Research
- Recent advancements in Staphylococci research
- Emerging therapies and vaccine development
- Case Studies
- Real-life examples of Staphylococcal infections and their management
- Conclusion
- Summary of key points
- The ongoing importance of research and awareness
- References
- Citations of relevant scientific studies, articles, and resources
This white paper would provide a thorough understanding of Staphylococci, ranging from their basic biology and classification to their clinical significance and current research efforts. It could serve as a valuable resource for healthcare professionals, researchers, and anyone interested in learning more about these bacteria and the challenges they pose in the field of medicine.